Let's take a deeper look into some of the most present health conditions and their surgical solution
As a surgeon with more then a decade of accumulated specialist experience stretching across two continents, while working in high-volume surgical departments, I strongly believe that it's crucial to share my clinical experience in order to offer a better insight into the most present health conditions which people are facing. In this first chapter, I'll be addressing the management of obesity, different surgical options and gastric balloon placement. But also, I will reflect on reflux disease, it's causes and treatment types. Last but not least, hernias are one the topics to be discussed in this blog chapter.
Once, we go through these topics, please be informed that Chapter II is to follow, reflecting on health conditions such as colorectal cancer, gallbladder stones, diverticulitis, appendicitis
Chapter I
Obesity, what are our options ?
It is estimated that obesity has tripled in human population in the past four decades. WHO data is showing that currently more then 600 million people are obese, and close to 2 billion people are overweight. So, the first question which comes to mind is what's the difference between being overweight and being obese ? The method used to explain the difference is the measurement of a Body-Mass-Index ( BMI ), which is a simple weight-for-height index. It is defined as a persons weight in kilograms divided by the square of his height in meters ( kg/m2 ). So therefore, overweight is a person whose BMI is greater then 25, while an obese person has a BMI equal or greater then 30.
Weight loss is one of the most searched topics online and a common goal for many people, whether it's for health reasons, to improve appearance, or simply to feel better. While there are many different approaches to weight loss, the key is to find a sustainable method that works for you. In this blog post, we'll explore some of the most effective strategies for achieving and maintaining a healthy weight.
First and foremost, it's important to understand that weight loss is not a quick fix or a one-time event. It requires a long-term commitment to healthy habits, including a balanced diet, regular exercise, and consistent self-care. With that in mind, there are several steps in the weight loss journey:
1. Set realistic goals about the amount of weight you want to lose, focus also on the timeframe in which you want to achieve that
2. Healthy eating, This means eating plenty of fruits, vegetables, lean protein, and whole grains, while avoiding processed foods, sugary drinks, and unhealthy fats. Consider working with a registered dietitian or nutritionist to create a personalized meal plan that meets your specific needs.
3. Exercise, get moving. The exercise that you stick to, is the one that will allow you to lose weight.
4. Well-being. It’s important to keep a positive mindset and a positive approach towards weight loss, as well as not giving up.
What if you are unable to lose weight, or you lose the weight, but only to regain it after some time. What is the solution for you ? It’s time for you to consult a bariatric surgeon. The decision for a patient to undergo bariatric surgery is very significant, and therefore the patients need to be fully informed and prepared.
The first step is an evaluation by a bariatric surgeon to determine the best treatment option for the patient. This evaluation includes a thorough review of medical history, physical examination, and a review of the patient's weight loss efforts to date. The surgeon will also discuss the different types of treatment and types of bariatric surgery and their potential risks and benefits.
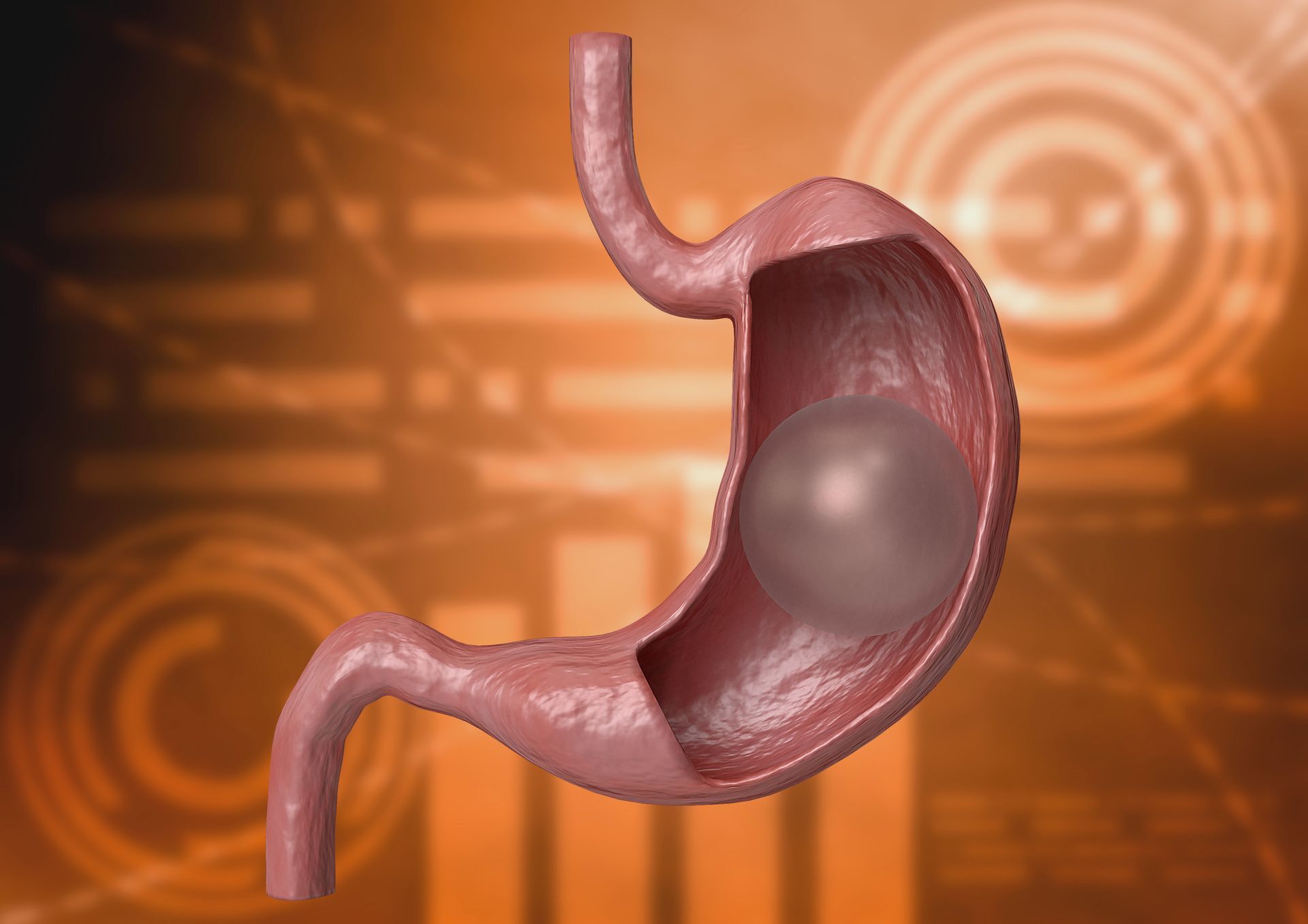
For some patients, placing a gastric balloon is a better fit. For example, patients that have a BMI between 27 and 35, have the option of having a gastric balloon placed for them. With this new method, where we are placing a swallowable gastric capsule-balloon in the stomach, the patient is able to lose 15% over the course of 4 months.
Patients with a BMI between 35 and 40, but with some comorbidities ( like hypertension, diabetes, polycystic ovary syndrome ), as well as patients with a BMI above 40, are prime candidates for bariatric surgery. In patients that are super obese ( BMI>50 ) there is an option inserting the patient with a gastric balloon first, as a sort of preconditioning them before performing the bariatric surgery. There are several different types of bariatric surgery:
1. Sleeve gastrectomy
2. Gastric by-pass
3. Mini gastric by pass
4. Adjustable gastric band
- Sleeve gastrectomy: involves removing a large portion of the stomach, leaving behind a smaller, tube-shaped stomach (approximately the size of a banana). This restricts the amount of food that can be consumed, leading to weight loss. During the sleeve gastrectomy, around 2/3 of the stomach volume is being removed, leaving behind a smaller, tube shaped stomach
2. Gastric by-pass: is a surgical weight loss procedure that involves creating a small stomach pouch and rerouting the small intestine to this new pouch. The procedure is typically done under general anesthesia and involves making several small incisions in the abdomen. A laparoscope, which is a small camera, is inserted through one of the incisions to allow the surgeon to see inside the abdomen. The stomach is then divided into a small upper pouch and a larger lower pouch. The small intestine is then rerouted to the new small pouch, bypassing most of the stomach and the upper portion of the small intestine
3. Mini gastric by-pass: is a surgical weight loss procedure that is similar to a traditional gastric bypass, but with some differences in the way the procedure is performed.In a mini gastric bypass, a small stomach pouch is created, similar to a traditional gastric bypass. However, instead of rerouting the small intestine to this new pouch, a longer segment of the small intestine is looped and attached to the stomach pouch.
4. Adjustable gastric band: a surgical weight loss procedure that involves placing an adjustable band around the upper part of the stomach, creating a small stomach pouch above the band. This restricts the amount of food that can be consumed, leading to weight loss. Although a temporary solution, gastric band has a benefit of adjusting the tightness on the upper part of the stomach and therefore, regulating the size of the stomach pouch, and the level of satiety that accompanies it.
If the patient is deemed as a good candidate for bariatric surgery, they will need to undergo a series of pre-operative tests and evaluations to ensure that they are healthy enough for the procedure. These tests may include blood work, imaging studies, and psychological evaluations.
Following their surgery, patients will be advised to adhere to a diet and exercise plan ( given to them by the dietitian ) as they continue their weight loss journey. This includes consuming small, frequent meals of high-protein, low-fat foods, and avoiding sugary or processed foods. It has also been shown that bariatric surgery improves or resolves many obesity-related health conditions such as type 2 diabetes, high blood pressure, and sleep apnea. Patients will also need to incorporate regular physical activity into their daily routine to help maintain their weight loss and improve their overall health, therefore allowing for the bariatric surgery to be a life-changing event.
it is important to remember that bariatric surgery is not a quick fix, and patients must be committed to making lasting lifestyle changes to maintain their weight loss over the long-term. By working closely with their medical team and adhering to a diet and exercise plan, patients can achieve significant weight loss and allow their bariatric surgery to be a life-changing event.
Is gastric balloon a good solution for obesity ?
There is an increasing demand for gastric balloon placement among patients that are struggling with weight loss. The procedure that is the most searched online and which generates the highest interest is the swallowable gastric pill balloon procedure. As a surgeon that's addressing weight loss in daily clinical practice, I feel obligated to share my thoughts and my clinical experience on this topic. Let us first get a better understanding of the procedure, indications, as well as, contraindications for this procedure.
The swallowable gastric pill balloon is a temporary gastric balloon that promotes weight loss in overweight and obese individuals. It is a gastric balloon (also known as an intragastric balloon or IGB) that is enclosed in a capsule and is swallowed by the patient to introduce the Balloon into the stomach. During swallowing, the proximal end of the Delivery Catheter remains outside of the patient’s mouth to permit filling. Once the Balloon position has been confirmed to be in the stomach via X-ray, the Balloon can be filled with the provided Filler Kit. After filling, the Delivery Catheter is removed from the Balloon by gently pulling back.
The filled Balloon is designed to remain in the stomach for approximately 16 weeks and reduce the weight by 10-15%. However, the duration of balloon residence, as well as the amount of weight lost during that time, may vary between individuals. During this time, the Balloon operates in the same ways as other IGBs ( inflatable gastric balloons )to promote satiety and reduce food consumption. The patient is supervised by a trained physician that will ensure at least a 4 follow-up visits during that period. At the end of the treatment period, the Balloon is designed to automatically open and drain. At this point, the empty Balloon is designed to transit the gastrointestinal tract and be excreted without further intervention. In rare cases, the drained Balloon may exit the stomach via vomiting.
Indications for the Balloon placement are to promote weight loss in overweight and obese individuals. In reference to the BMI range, all patients above the BMI of 27 can have the balloon placed. The balloon can also be placed for the patients with the BMI above 40, eventhough for these patients, bariatric surgery is a more suitable approach for weight loss. In patients with BMI above 40 ( even the super obese patients with BMI above 50 ), the balloon can be placed in either of the following two situations:
1. If a patient is reluctant to go for bariatric surgery or
2. If it’s a super obese patient ( BMI above 50 ), in which case the aim is to reduce the weight, in order to precondition them for the following bariatric surgery. The preoperative weight loss can leads to a reduced chance of postoperative complications.
What about contraindications ? Who does not qualify for the balloon placement ?
- Patients that underwent any kind of bariatric surgery ( sleeve gastrectomy, by-pass, gastric band )
- Patients with severe dysphagia
- Patients with a large in size hiatal hernia, that are on proton pump inhibitor therapy
- Severe coagulopathies and liver disease
- Pregnancy or desire to become pregnant during the course of 4 months
- Gastric ulcers, which can result in bleeding or perforation
- Alcoholism or drug addiction
So, as we can see, there are clear guides as to who is/isn't eligible for the gastric balloon placement. In addition to the previously mentioned 7 groups, there is one more group of patients that are not eligible for the balloon placement. Some people are just looking to shave off extra 5-10 kg and to achieve the perfect beach look, and even though they are not overweight or are slightly overweight ( BMI<27 ), they are looking to have the balloon placed. These patients should be given advice and a diet plan from a trained dietitian, but if by any chance they arrive to a surgical clinic, it is absolutely necessary that the surgeon clearly explains that they do not qualify for this procedure.
Recommendations after the IGB placement are as follows:
- Patient should be on prophylactic PPI therapy ( proton pump inhibitors )
- Daily multivitamin supplementation with 1 to 2 adult doses
- Antiemetic regimen ( to take medication to combat nausea ) for 2 weeks following the placement
What can a patient expect following a balloon placement ? In my clinical experience, it is absolutely crucial that a surgeon dedicates optimal time and effort in explaining the procedure itself, possible complications, but also what can a patient expect after the first couple of days following the balloon placement. Now you may ask, well don't you do that before every procedure ? The answer is, of course, YES. But there is one key difference to take note of. Because this procedure doesn't require anaesthesia, and is an out-patient procedure, it is possible that the patient might have a preconceived idea that there are no symptoms present following the balloon placement. Although the symptoms are not present always, it is possible that some of the patients might experience pain ( in the form of stomach cramps ), nausea and vomiting. These symptoms usually start 6-12h after the balloon has been placed and last for 3-4 days. If a patient experiences these symptoms, he/she are given pain relief ( oral or intravenous ), as well as previously mentioned proton pump inhibitors and anti-emetics ( medication against nausea ). Usually, after 5-7 days, patients are eligible to start with physical exercise. There is one more important point to make. Gastric balloon is not a magic pill, but it's a good tool for the patients that are willing to make a shift in their life. The concept of a gastric balloon placement is not just for the patient to have a temporarily ( 16 weeks ) reduced stomach volume that can take up less food, but also for the patients to change their diet during that process, which can lead to satisfying long term results.
What is the conclusion ? When indicated, the swallowable gastric pill balloon is a good solution for weight loss, it is safe, fast and offers the least amount of discomfort for the patient.
Reflux and Heartburn; For how long can I take medication, do I need Anti-reflux surgery ?
Complaints of heartburn are one of the most frequent health conditions which brings the patient to a doctor's clinic. More often then not, I witness the stories of patients visiting my clinic after they have been taking Proton Pump Inhibitors ( PPI ) for years, as a solution for their heartburn. The main question that come to mind, does long-term PPI therapy solve the problem? The answer to that question is NO. The second question is related to the safety of long term PPI use. Heartburn occurs as a result of gastro-oesophageal reflux ( GERD ), or just "reflux", as it's referred to by many.
Gastroesophageal reflux disease (GERD) is a chronic condition in which acid from the stomach flows back ( reflux ) into the esophagus, causing symptoms such as, previously mentioned, heartburn, chest pain, and difficulty swallowing. GERD affects millions of people worldwide and can significantly impact a person's quality of life if left untreated. The typical finding in a case of GERD is a weakend Lower Esophageal Sphincter ( LES ). Causes of GERD are multiple, such as obesity, pregnancy. Both of these conditions are accompanied by an increased intraabdominal pressure, which is favourable for LES hypo function. Also, smoking and certain types of food ( spicy or fatty food ) are the causes of functional weakening of the LES. But the most common condition that causes a LES hypo function and reflux, is the existence of a Hiatal hernia.
Hiatal hernia constitutes of a portion of the stomach ( or the entire stomach ) pushing through the diaphragm opening ( Hiatus ) into the chest cavity. In some cases, apart from the stomach, several other intraabdominal organs can pass through this opening, therefore creating a large in size hernia. There are four different types of hiatal hernias:
- Sliding: the most common one, occurs in 95% of the cases, when there is a displacement of the LES into the chest cavity
- Paraesophageal: LES is in place, but the stomach fungus is pushing through the hiatus and into the chest cavity.
- Mixed type: this type is basically a combination of the first and second type
- It is also a mixed type, but apart from the stomach, an additional organ/or organs are through the hiatus and into the chest cavity
What are the most common symptoms of GERD ? I have already mentioned Heartburn ( a burning sensation, or pain felt in the chest after taking a meal or when lying down. Other symptoms are:
- Regurgitation: A bitter or sour taste in the mouth, often accompanied by the sensation of food going back into the throat.
- Difficulty swallowing: A feeling of food getting stuck in the throat or chest.
- Chest pain: Pain or discomfort in the chest, sometimes mistaken for a heart attack.
- Chronic cough: A persistent cough, often worse at night.
- Hoarseness or sore throat: Irritation of the vocal cords caused by acid reflux.
How do we diagnose GERD ? WE can highly suspect that there is presence of GERD based on a person's symptoms, but further testing are necessary to confirm the diagnosis and rule out other conditions. Tests that are used to diagnose GERD include:
- Upper endoscopy: A flexible tube with a camera on the end is inserted through the mouth and into the esophagus to check for clear signs of reflux ( zone of inflammation or damage of the mucosal layer ) and the existence of a hiatal hernia.
- Esophageal pH monitoring: A small device is inserted through the nose and into the esophagus to measure the amount of acid present.
- Esophageal manometry: A small tube is inserted through the nose and into the esophagus to measure the pressure and strength of the esophageal muscles.
What is the significance of these tests ? In patients that don't have a hiatal hernia and present on the endoscopy with clear signs of reflux, the next step is to perform an Esophageal manometry, which is used to localise and analyse the LES ( lower esophageal sphincter ) function, as well as the muscle tone and contractions of the esophagus. However, if patients have no abnormalities recorded of the manometry, they are advised to opt for pH monitoring test, which allows the physician to detect pathological exposure of the esophagus to stomach acid.
What about treatment of GERD ? If you remember, at the start of this blog two questions were highlighted regarding the safety and effectiveness of long term PPI use in combating GERD. So, does the long term use of PPI's solve the problem of GERD ? The answer to that question is NO. The second question is related to the safety of long term PPI use and the concerns of possible links to an increased risk for stomach pathology, vitamin B12 malabsorption, hypomagnesemia etc. There is not enough data to establish a definitive link between long term PPI use and these adverse effects, but it does highlight the necessity to thorough approach to the causes of GERD and consequently the treatment options.
A laparoscopic fundoplication is a minimally invasive procedure that is used as a surgical solution for GERD in patients that have a diagnosed hiatal hernia or a diagnosed hypo functioning LES ( Lower oesophageal sphincter ).
During a laparoscopic fundoplication, several small incisions (5-10mm) are made on the abdominal wall and are used to insert a camera and light, and other specialized instruments. The upper part of the stomach, called the fundus, is wrapped around the lower end of the esophagus, creating a tight valve that prevents stomach acid from flowing back into the esophagus. If there is a herniation of the stomach, the stomach needs to be surgically repositioned from the chest cavity into the stomach, and the defect on the diaphragm needs to be repaired with sutures or with a mesh ( depending on the size of the defect ). Once the defect has been repaired, fundoplication can follow. This procedure is typically performed under general anesthesia and takes about 1-2 hours to complete. Compared to traditional open surgery, laparoscopic fundoplication typically involves less pain, scarring, and a shorter recovery time.
Following the surgery, patients are advised to follow a DIET PLAN that is catered towards preserving the surgically created valve mechanism, ensuring the long term success of the performed procedure.
What about hernias, symptoms, types and treatment ?
We can safely say that the very existence of hernias goes back through multiple millenniums. Hernias were first documented in papyrus scrolls from ancient Egypt that date back to about 1550 BC. These scrolls addressed a variety of medical conditions, including hernias. The physician Hippocrates (460–370 BC) provided a thorough description of inguinal hernias and their treatment in the ancient Greek literature on hernias. In his medical writings, the Roman physician Celsus (25 BC–50 AD) extensively discussed hernias, outlining their symptoms and indicators as well as possible treatments.
Over the centuries, the understanding and treatment of hernias continued to evolve. The renowned anatomist Andreas Vesalius gave information on the anatomy of the abdominal wall and hernia causes in the 16th century. In the 19th century, surgical techniques for repairing hernias were refined, and by the early 20th century, hernia surgery had become a common procedure.
So, have do we define hernias in this modern age ? We say that a hernia is a condition that occurs when an organ or tissue pushes through a weak spot in the muscle or tissue that normally holds it in place. This can happen in various parts of the body, but the most common types of hernias occur in the abdominal area. What are the common types of hernia ?
- Inguinal hernia : Considered to be the most common type of hernia existing in the human population, defined as a protrusion of an intraabdominal organ or structure through a abdominal wall weak spot in the groin ( inguinal) region.
- Umbilical hernia : Occurs when an intraabdominal organ or structure ( such as fatty tissue ) protrude through a abdominal wall weak spot in the umbilical ( bellybutton ) region.
- Incisional hernia : also often classified as a postoperative hernia, it's a abdominal wall defect that is at the site of previous surgical incision (surgical scar)
- Hiatal Hernia : happens when a part of, or the complete stomach pushes through the opening on the diaphragm and into the chest cavity. We will mention more about hiatal hernias in detail in our following blog on GERD (gastro-oesophageal reflux disease)
The most common symptom that is related to the existence of a hernia is pain. Pain is usually increasing while there is some physical activity being performed ( such as bending, lifting heavy objects or gym workouts ). It's important to note that hernias are accompanied by a visible bulge, which becomes more prominent when that region is exposed to an increased pressure ( achieved during lifting objects, running, workouts etc. ).
What about the treatment of hernias ? Well, it's a straight forward answer-surgery. Today, the advancements in technology and it's implementation in every day surgical practice, have drastically improved the long term outcome and the recovery time for patients undergoing hernia surgery. What do we mean by technological advancements ? Let's just highlight several of them. First, the invention and implementation of a mesh in reinforcement of the weakend abdominal wall, has greatly reduced the rate of hernia reoccurrence. Surgical meshes have undergone significant evolution and development over time, leading to the creation of more effective and safer products. So, how have the surgical meshes evolved ? Let's take a look:
- Materials: Once constructed of animal tissues like pig or cow intestines, surgical mesh has since been created of synthetic materials including polypropylene, polyester, and ePTFE (expanded polytetrafluoroethylene). More resilient, less prone to infection, and less likely to be rejected by the body are synthetic meshes.
- Design: Surgical mesh designs have also changed over time. Meshes were originally flat and basic, but they are now offered in a variety of sizes, forms, and features, such as multiple layers, adjustable tension, and reinforced edges. These adjustments have made it possible to position the weakening abdominal wall in a better location and with better support.
- Biocompatibility: Since the advent of coatings that encourage tissue ingrowth, lessen inflammation, and lower the risk of infection, surgical meshes have become more biocompatible.
- Laparoscopic mesh placement: As a result of the development of laparoscopic surgery, it is now possible to implant surgical meshes through tiny incisions, causing less tissue damage, a quicker recovery, and fewer difficulties.
- 3D printing: The use of 3D printing technology has made it possible to create personalized meshes that are sized and shaped to precisely match the demands of the patient, leading to better results and fewer issues.
We mentioned laparoscopy. I'm sure that by now, that the vast majority of people that have ever searched online about surgical treatment have come across the phrase "laparoscopic". Well, the word comes from the Greek words "lapara" meaning "flank" and "skopein" meaning "to see". Laparoscopic hernia treatment has become the gold standard, reflecting both the recovery, as well as the long term results. So, how is it done exactly ? Laparoscopic procedures are performed through small in size incisions on the abdominal wall, ranging from 5-10mm, with major emphasis on the ergonomics of the ports, which enables me to have the optimal utilisation of the surgical instruments needed for successful and long lasting positive outcome of the performed surgery.
In 10 years of specialist practice ( both in the UAE and Serbia ) I have strived for excellence in laparoscopic hernia management. I am offering the full range of laparoscopic hernia management ( inguinal, postoperative, umbilical and hiatal ) as a daystay procedure in more then 90% of the cases.
What is my preferred treatment of choice for hemorrhoids ?
The THD Procedure: A Game-Changer for Hemorrhoid Treatment
Transanal Hemorrhoidal Dearterialization (THD) has revolutionized the management of hemorrhoids, offering patients a safe, effective, and minimally invasive alternative to traditional hemorrhoidectomy. By addressing the root cause of hemorrhoidal symptoms—excessive blood flow to the hemorrhoidal plexus—THD achieves symptomatic relief with minimal discomfort and downtime.
What is THD?
THD is a Doppler-guided procedure that targets the arterial blood flow feeding the hemorrhoids. Using a specialized probe, the surgeon identifies and ligates the arteries, reducing blood flow and allowing the hemorrhoidal tissue to regress naturally. Unlike excisional hemorrhoidectomy, THD avoids cutting or removing tissue, preserving the anatomy of the anal canal and reducing postoperative complications.
Key Benefits of THD
- Minimally Invasive Technique: THD involves no tissue excision, significantly reducing pain and discomfort compared to traditional surgeries.
- Quicker Recovery: Most patients can return to their normal routine within a few days, with minimal disruption to daily life.
- Low Risk of Complications: The procedure minimizes bleeding, infection, and other common surgical risks.
- Preservation of Anatomy: THD maintains the structural integrity of the anal canal, reducing the likelihood of long-term complications like fecal incontinence.
- Versatility: THD is effective for treating both internal and mixed hemorrhoids across various grades, making it a suitable option for a wide range of patients.
The Role of Training and Education
While THD is highly effective, its success depends significantly on the expertise of the surgeon. Proper training and education in this field are essential to mitigate intraoperative risks and optimize postoperative outcomes.
Comprehensive training programs familiarize surgeons with the Doppler-guided technique, ensuring accurate identification and ligation of hemorrhoidal arteries. This reduces the risk of incomplete dearterialization or inadvertent damage to surrounding tissues, which could lead to complications or symptom recurrence.
Additionally, education emphasizes postoperative management strategies to monitor patient recovery effectively. Understanding potential issues, such as mild discomfort or rare recurrence, enables timely interventions that enhance patient satisfaction.
Key takeaways
THD represents a paradigm shift in the treatment of hemorrhoids, offering superior outcomes with minimal pain and downtime. By prioritizing proper training and continuous professional development, surgeons can harness the full potential of this innovative technique. As more healthcare professionals adopt THD, it has the potential to become the gold standard in hemorrhoid treatment, providing patients with effective, safe, and lasting relief.
Interested in these topics? Don't hesitate to reach out to dr Alex for more information!
We want to know your needs exactly so that we can provide the perfect answer. Let us know what you want and we’ll do our best to help.